A physiotherapist has given an inaugural lecture at the doctoral college of the University of Leicester, after being invited to speak on the subject of her award-winning PhD.

Clinical academic Emma Jones
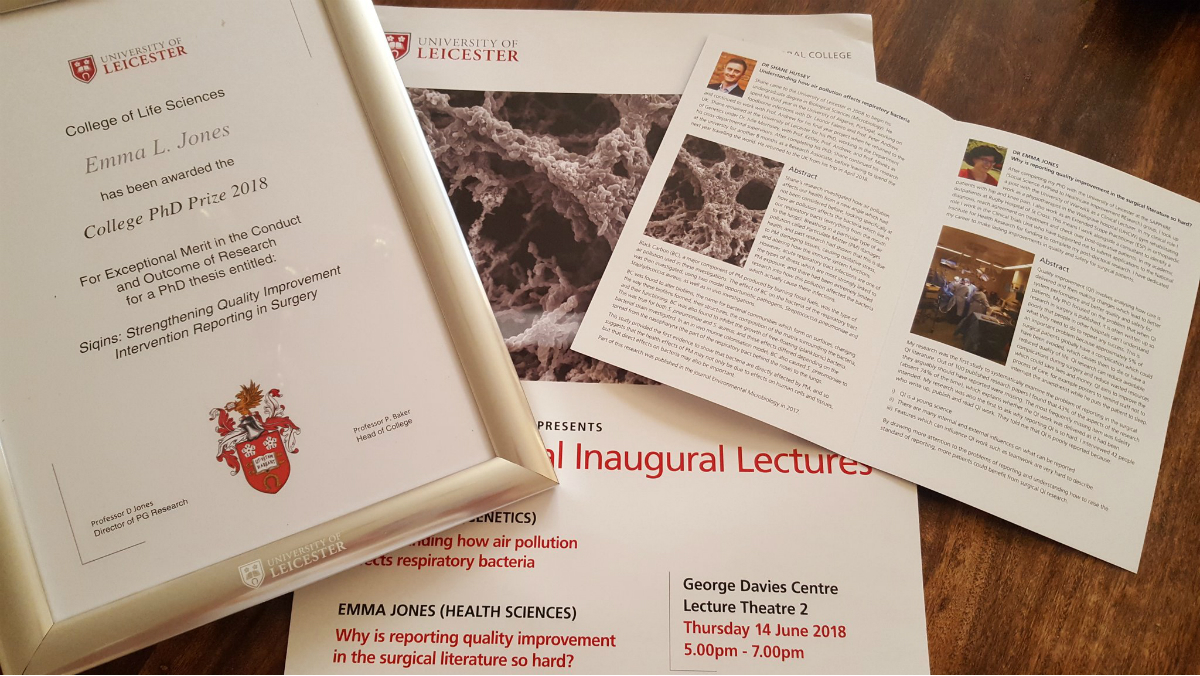
Emma Jones received an award for PhD excellence from the university’s College of Life Sciences for her thesis, titled Strengthening quality improvement intervention reporting in surgery.
The lecture, held on 14 June and available on YouTube, was presented to an audience of academics, clinicians and members of the public.
Dr Jones, who is now a clinical academic at the University of Warwick, told Frontline: ‘Quality improvement (QI) involves analysing how care is delivered and then making changes, which lead to better system performance and better quality and safety for patients.
‘But when QI research in surgery is published, it is often written up so poorly that people in other hospitals can’t understand what they need to do to repeat any success. Elements are frequently missing, which means the research is not replicable.
‘This is an important problem because approximately five per cent of surgical patients globally have a complication, which could have been avoided, which causes them to die or have a reduced quality of life.
‘QI research can reduce avoidable complications during surgery and reduce wasted resources, which could save lives and money. It aims to improve the process of care, for example by using posters to remind staff not to interrupt the anaesthetist while he puts a patient to sleep.’
Social interventions can be hard to measure
Dr Jones PhD research at Leicester was the first study into why reporting QI is difficult, and involved a systematic review of related surgical literature.
‘Out of 100 published research papers, I found that 43 per cent of the aspects of research that they should have been reporting were missing,’ she said.
‘The most frequently missing item was fidelity - which was absent 74 per cent of the time. Fidelity explains whether the quality improvement work was delivered as it had been intended.’
During her PhD, she interviewed 42 people who wrote, read and publish QI reports. They included physiotherapists, radiographers, pharmacists, anaesthetists, nurses and surgeons. Their feedback indicated that poor reporting could be due to a number of factors, including
- Difficulty in measuring social interventions, i.e. describing features that can influence QI work, such as workplace culture, teamwork or leadership
- Institutional pressures, e.g. clinicians lacking time and resources to learn how to conduct good quality improvement work
- Conflicts of interest and internal and external influences on what can be reported
A toolkit to improve reporting
Dr Jones is now applying for funding to develop a toolkit to help clinicians to improve their QI reporting.
‘By drawing more attention to the problems of reporting and understanding how to raise the standard of reporting, more patients could benefit from surgical QI research,’ she said.
Author: Robert Millett
Number of subscribers: 0